In Mozambique, a teenage rape victim sought care at a health clinic only to find it closed. In Zimbabwe, Aids-related deaths have risen for the first time in five years. In Ethiopia and the Democratic Republic of the Congo (DRC), patients with suspected HIV went undiagnosed due to test-kit stocks running out.
Stories of the devastating impact of US, British and wider European aid cuts on the fight against HIV – particularly in sub-Saharan Africa – continue to mount as 2025 comes to an end, and are set out in a series of reports released in the past week.
The Trump administration abruptly cut all overseas aid spending in January, with only piecemeal restorations to funding since then. Other countries, including the UK, have announced their own cuts. It has been estimated that external health assistance over 2025 will be between 30% and 40% lower than it was in 2023.
Winnie Byanyima, USAID’s executive director, said: “The complex ecosystem that sustains HIV services in dozens of low- and middle-income countries was shaken to its core.”
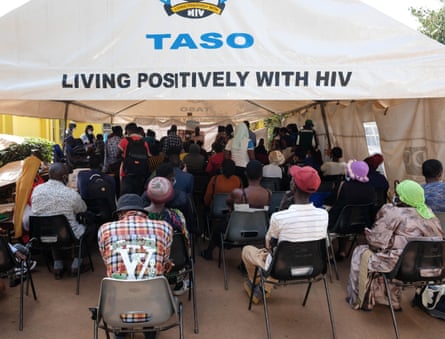
Without swift action to get services back on track, UNAids has predicted there will be 3.3m more new HIV infections by 2030 than expected. And while there are signs of recovery, including new domestic funding in some countries, access remains far from universal.
The UN agency’s report finds that services working to prevent HIV infections were particularly likely to be donor-funded and are among the hardest hit – with resources limited, treatment for existing patients has been prioritised. In Burundi, for example, the number of people receiving preventive HIV medicines fell by 64%.
A separate series of country-level reports from the British charity Frontline Aids, covering Angola, Kenya, Malawi, Mozambique, Nigeria, Tanzania, Uganda and Zimbabwe, highlights similar issues.
The full figures will take time to collate, but in some places there are already signs that new HIV cases, or Aids-related deaths, are rising after years of heading downwards.
Many of the gains in the fight against HIV in recent years have come via the recognition that some groups of people are at higher risk of infection – known as “key populations”. They include men who have sex with men, people who inject drugs, sex workers, transgender people, and prison inmates.
In each case, offering services specifically designed around those groups’ needs has borne fruit – for example, LGBTQ+ friendly walk-in clinics can mean access to care for people who are stay away from public clinics due to the stigma around HIV.
Many of those clinics and other outreach services have closed, along with swathes of community-led organisations, previously reliant on donor funding. One member of the LGBTQ+ community in Uganda, quoted in the Frontline Aids country report, said the loss of safe spaces had left them “isolated and exposed […] the mental strain is overwhelming”.
In sub-Saharan Africa, teenage girls and young women are disproportionately affected by HIV, but programmes designed specifically for them are another common casualty of the cuts.
In Kenya, activists report that people who can do so are hiding the fact they belong to a key population so as to access care in public clinics safely. They fear this will mean a loss of information on where and how the virus is spreading.
John Plastow, executive director at Frontline Aids, said: “We are already seeing progress slip backwards.”
But Plastow also saw the potential for a reset of health policies. “In several countries,” he said, “we are seeing the first signs of governments and communities working together to build more sustainable, homegrown HIV responses.”
UNAids also pointed to signs of hope, with countries including Nigeria, Uganda, Côte d’Ivoire, South Africa and Tanzania all pledging to increase domestic investment.
And, they said, innovations such as new long-acting injectable drugs to prevent infection were “gaining momentum”.
“We know what works – we have the science, tools and proven strategies,” said Byanyima. “What we need now is political courage: investing in communities, in prevention, in innovation and in protecting human rights as the path to end Aids.”