Published: | Updated:
It’s one of the most common forms of cancer in men, yet too many do not know the crucial warning signs to look out for, a leading cancer surgeon has warned.
Whilst many men find discussing this topic uncomfortable, the fact remains that one man dies every 45 minutes from prostate cancer in the UK alone.
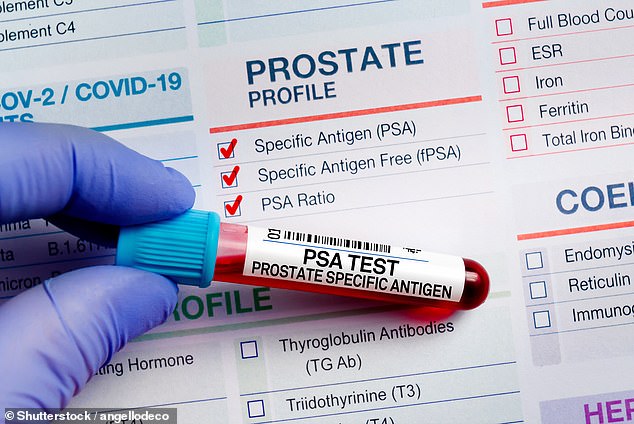
And while the risk of prostate cancer increases with age, Mr Tim Dudderidge, a consultant urological surgeon and lead of prostate cancer trials at University Hospital, Southampton, advises all men to request a prostate specific antigen (PSA) test from their GP once they reach their fiftieth birthday.
Mr Dudderidge told the Daily Mail: ‘The reason we are so keen on screening programmes is that fundamentally this is a disease that arises in its most lethal and most curable phase at a time when you don’t typically have symptoms.’
The prostate is a small gland that sits just below the bladder and produces part of the fluid present in semen.
Despite being the second most common form of cancer in men – with more than 63,000 cases diagnosed every year – it is one of the most misunderstood forms of the disease.
In its earliest stages, prostate cancer is usually symptomless, which helps explain why so many men are only diagnosed once the disease has progressed and when their prognosis is much more bleak.
Figures suggest that over 45 per cent of men do not know that it can present without physical symptoms, meaning that a huge number of men not diagnosed until it’s too late.
According to research carried out by Prostate Cancer UK, only a third of men realise that it can be present with no physical symptoms, prompting doctors to push for men to proactively understand their risk factors.
One of the most worrying beliefs when it comes to prostate cancer, experts say, is that people seem to believe it’s one of the ‘good ones’, because it’s not deadly.
But Mr Dudderidge says this cannot be further from the truth. In fact, more than 12,200 men die a year from the disease, with one in eight receiving a diagnosis in their lifetime.
Contrary to popular belief, whilst difficulty passing urine can be a symptom of non-cancerous problems, such as an enlarged prostate, it is not usually a symptom of prostate cancer, at least in its early stages.
Needing to go more frequently or with more urgency can also just be a sign of getting older, but Mr Dudderidge advises if something doesn’t feel right, it is always best to consult your doctor.
The signs of more advanced prostate cancer can present as unexplained weight loss, fatigue and back or bone pain that doesn’t go away.
Deep pain or stiffness in the lower back, hips or upper thighs are some of the most commonly overlooked symptoms, Mr Dudderidge said.
This can be a sign that the cancer has spread, but is often dismissed as simply part of getting older, or muscle injury.
Mr Dudderidge added: ‘A sudden onset of difficulty getting or keeping an erection, without another clear cause like stress, can sometimes be a sign, as can blood in the semen.
‘Men often ignore this if it happens only once, but it should always be checked.’
Whilst most men under 50 are unlikely to develop prostate cancer, there are a number of risk factors men need to be aware of, Mr Dudderidge says.
Men of black descent are around twice as likely as white men to develop the disease and die from prostate cancer.
Having close family members with prostate, breast or ovarian cancer, or carrying the BRCA1 or BRCA2 gene variant, also puts men at greater risk of the disease. As such, these men are advised to start testing from the age of 45.
After a PSA test, if doctors are still concerned, patients may be scheduled for an MRI and consequently a transperineal biopsy – a procedure to remove tissue samples from the prostate gland – to check for cancer cells.
Treatment for prostate cancer depends on how early it’s caught and how fast it is likely to grow.

On Friday 28th November, the National Screening Committee (NSC) said there was not enough evidence that testing all men for prostate cancer would save a substantial number of lives.
As about half of prostate cancers are slow growing – so they pose little threat to health – the NSC said screening all men at a certain age could lead to unnecessary anxiety and treatment. Instead, they proposed that men with a BRCA gene mutation – which is linked to a higher risk of prostate cancer – should be screened every two years from age 45 to 61.
It is thought that up to 30,000 men would qualify – however, few will know they have the variant as most men are not gene tested.
The decision will be subject to a public consultation.
The main treatments include surgery, radiotherapy and hormone treatment, but for many with early stage prostate cancer immediate treatment is not always needed.
Rather, doctors will offer active surveillance, which means regular tests and screening to monitor the cancer closely, without having to perform unnecessary surgery which can lead to impotence and incontinence.
At this stage, when the disease is caught early, more than 85 per cent of men will live for at least ten years after their diagnosis, according to Cancer Research UK.
‘The only way to give everyone a fair chance, and to keep this number up, is to develop a routine screening programme,’ Mr Dudderidge said.
It comes as a panel of expert government health advisers announced last week that prostate cancer screening should not be made available to the vast majority of men across the UK – to the ‘deep disappointment’ of several charities and doctors.
The UK National Screening Committee instead recommended that there should be a targeted screening for men with the faulty gene variants, which means that are at higher risk of faster growing and aggressive cancers at a younger age.
The committee added that the ‘harms would outweigh the benefits,’ if it were to recommend prostate cancer for all men, resulting in ‘very high levels of over-diagnosis.’
In response, Mr Dudderidge is now urging men to educate themselves about the risks of both the disease and getting tested, in a bid to keep prostate cancer deaths down.
He said: ‘Essentially men need to make themselves aware—and if they decide they do want testing, and they can accept the downstream risks of testing—the NHS should still honour that.’
‘Men can also get at home testing kits, which give a binary answer, but that might also help.
‘It’s also not completely out of reach to get a private MRI scan to detect significant disease – the cancers that are posing the greatest threat of spreading. Unfortunately the PSA test does not deliver these same results.
‘In the meantime, I advise all men to read up and understand the pros and cons of the screening and the treating process.
‘We are making efforts on all these fronts – using the least invasive testing methods and robotic surgery which allows men to keep their erections – to show that screening saves lives without too many side effects.
‘Currently, there are too many men dying of this disease and that’s what keeps me going every day with the work we do.’
Laura Kerby, the chief executive of Prostate Cancer UK, said the decision came as a ‘blow to the tens of thousands of men, loved ones and families who’ve fought for a screening programme’.
She added: ‘While screening men with BRCA gene variations will save only a fraction of that, the committee’s decision is the first time they’ve recommended screening of any kind for prostate cancer. It shows that research and evidence can shift the dial and save men’s lives.’
A huge clinical trial involving 300,000 patients – called Transform – has now started to try to fill gaps in the evidence on how screening could be safely rolled out to other groups, including those with a family history and black men.
Professor Hashim Ahmed, chair or urology at Imperial College Healthcare NHS Trust and study lead, said the recommendations were based on a ‘solid piece of work’ and that while some men will be disappointed, he felt the right decision had been made.
‘There is a small benefit… but the harms of diagnosing, testing and treating very much outweigh those benefits.’
The first results of the trial are expected in two years.








