By ELEN JOHNSTON – HEALTH REPORTER
Published: | Updated:
A new study has revealed fatigue, anxiety and pain are little known signs of multiple sclerosis (MS) that can strike 15 years before more well-known symptoms.
Typical symptoms of the autoimmune condition include difficulties walking, vision problem, numbness and muscle cramps.
The latest analysis looked at the health records of 12,000 people, tracking physician visits in the 25 years leading up to the onset of MS symptoms.
It was the first study to examine healthcare usage this far back into a patient’s clinical history.
They found a steady increase in the number of visits to a GP as early as 15 years before neurological symptoms set in.
This included an increase in visits to physicians for symptoms like fatigue, pain, dizziness, anxiety and depression.
The visits to psychiatrists for mental health problems specifically increased 12 years before.
But the researchers cautioned that not everyone who has these symptoms will go on to get the debilitating condition.

They also found visits to neurologists and ophthalmologists—also known as eye doctors—for blurry vision or eye pain increased eight to nine years before.
Then they saw an increase in visits to emergency and radiology departments three to five years before.
And finally, they observed an increase in visits to specialist physicians like neurologists a year before.
These patterns show signs ‘something is happening beneath the surface’ before it declares itself as MS, said Dr. Marta Ruiz-Algueró, a postdoctoral fellow at UBC, the study’s first author.
The earliest signs they observed ‘can be easily mistaken for other conditions’, warned Dr Helen Tremlett, professor of neurology at UBC’s faculty.
They believe their findings ‘dramatically shift the timeline for when these early warning signs are thought to begin’.
And they potentially open the door to opportunities for earlier detection and intervention, added Dr Tremlett.
Previously other researchers had found symptoms that appear five years before, such as constipation, urinary tract infections, and sexual problems.
MS is a life-changing, incurable condition affecting the brain and spinal cord that causes debilitating muscle spasms, among other symptoms.
While MS does not directly kill, at advanced stages, it can cause weakness in the chest muscles, leading to difficulty breathing and swallowing—which can have life-threatening complications.
Those in the late stage of the illness are also extremely vulnerable to potentially deadly infections.
Some studies show that MS patients are up to 75 per cent more likely to die young than those without the disease.
Most people find out they have MS in their thirties and forties, but the first signs can start years earlier.
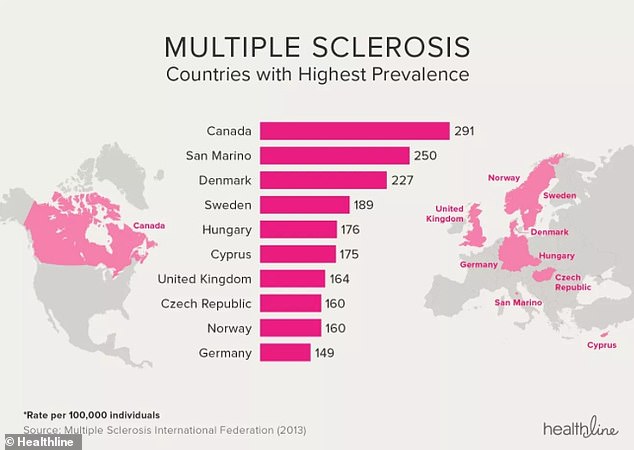
The latest study comes amid a concerning rise in cases, with around 150,000 people living with MS in the UK.
This is up from around 130,000 in 2019, according to recent research by the MS Society.
While experts don’t know the reason cases are on the rise, possible factors are infections, a lack of vitamin D, smoking, solvents, obesity, and stress.
It is important to spot the early signs of the condition, as while there is no cure for MS, treatments can slow the progression of the disease.
The type of treatment you will need depends on the type of the disease patients have: relapsing remitting, secondary progressive, and primary progressive.
Relapse and remitting MS involves flare-ups of symptoms where they get worse (relapse) and get better (remission).
Over time it often develops into secondary progressive MS, when symptoms are there all the time, and get slowly worse.
In the less common case of primary progressive MS, symptoms slowly getting worse over time without periods of them going away or getting better.
Treatments may include several types of medication such as steroids, disease-modifying therapies, muscle relaxants, and those to treat pain and other symptoms.
Other types of support include advice on fatigue, physiotherapy, mobility equipment, talking therapies, and cognitive rehabilitation.








